[ad_1]
I’ve written many articles detailing the roles vitamin D plays in COVID-19, from how it can help prevent initial infection, to how it can reduce your risk of complications and death. One of the reasons I’ve been pushing for vitamin D optimization as a way to minimize the risks associated with this infection is because the evidence for it is overwhelming.
British Health Authorities Disparage Vitamin D Claims
British health authorities, however, disagree.1 According to new COVID-19 guidance2 from the National Institute for Health and Care Excellence (NICE), Public Health England and the Scientific Advisory Committee on Nutrition (SACN), there’s insufficient evidence to support the recommendation to take oral vitamin D for the sole reason of preventing or treating COVID-19.
With that, they are backtracking on previous recommendations issued by British health officials who, in November 2020, urged people to take supplemental vitamin D this winter to reduce their risk of respiratory infections, including COVID-19.3
What’s more, while the new guidance does urge Britons to take a vitamin D supplement between October and March, it only recommends a dose of 400 IUs a day, which is easily 10 times lower than what most people would require for general health and immune function.
While the panel agreed low vitamin D was associated with more severe COVID-19 outcomes, they claim it’s impossible to confirm causality due to inconsistencies between the studies (such as dosing, setting, populations, duration and definitions of outcomes), and because vitamin D deficiency and severe COVID-19 share many of the same risk factors.
According to professor Ian Young, who chairs SACN, “This evidence review confirms that currently there is not enough available evidence to determine that there is a causal relationship between vitamin D and COVID-19.”
However, if vitamin D deficiency and COVID-19 share the same risk factors, wouldn’t it make more sense to urge people to address their vitamin D deficiency instead of using this as a justification for why vitamin D supplementation cannot be recommended?
It’s really hard to imagine that scientists with a genuine concern for public health would come out with this kind of guidance, especially when you consider that vitamin D supplementation — at whatever dosage required to get your blood level above 40 ng/mL (100 nmol/L) — won’t make your health any worse. There’s absolutely no downside to it.
Vitamin D Is Important for Optimal Immune Function
In the video above, Dr. Roger Seheult reviews how vitamin D works, and the benefits of vitamin D, both for respiratory infections in general and as it pertains to COVID-19.
Importantly, vitamin D is a steroid hormone that can pass through cellular membranes into the nucleus and controls the expression of genes. So, it’s not just a mere vitamin required as a cofactor. It can actually modify how the cells in your body behave and function.
Vitamin D receptors are found in a large number of different tissues and cells, including your immune cells. This means vitamin D plays an important role in your immune function specifically. If vitamin D is lacking, your immune system will be impaired, which in turn makes you more susceptible to infections of all kinds. As noted by Seheult, vitamin D:
- Stimulates “the innate immune response, which provides frontline protection against infectious agents”
- Increases expression of antimicrobial peptides in your monocytes and neutrophils — both of which play important roles in COVID-19
- Enhances expression of an antimicrobial peptide called human cathelicidin, “which is of specific importance in host defenses against respiratory tract pathogens”
Vitamin D for COVID-19
While Seheult also reviews a number of studies looking at vitamin D in relation to respiratory illnesses other than COVID-19, SARS-CoV-2-specific investigations have found:
• COVID-19 is far more common in vitamin D deficient individuals — In one study,4,5,6 82.2% of COVID-19 patients tested were deficient in vitamin D, compared to 47.2% of population-based controls. (Mean vitamin D levels were 13.8 ± 7.2 ng/ml, compared to 20.9 ± 7.4 ng/ml in controls.)
They also found that blood levels of vitamin D inversely correlated to D-dimer levels (a measure of blood coagulation). Many COVID-19 patients have elevated D-dimer levels, which are associated with blood clots.
• Vitamin D status influences COVID-19 severitys — COVID-19 patients who have higher vitamin D levels tend to have milder illness and better outcomes. One study7,8 found the risk of severe COVID-19 and related deaths virtually disappeared when vitamin D levels were above 30 ng/mL (75 nmol/L).
In another study,9 COVID-19 patients with a vitamin D level between 21 ng/mL (50 nmol/L) and 29 ng/mL (75 nmol/L) had a 12.55 times higher risk of death than those with a level above 30 ng/mL. Having a level below 20 ng/mL was associated with a 19.12 times higher risk of death.
My scientific review,10 “Evidence Regarding Vitamin D and Risk of COVID-19 and Its Severity,” published October 31, 2020, also lists data from 14 observational studies that show vitamin D blood levels are inversely correlated with the incidence and/or severity of COVID-19.
This makes sense when you consider that vitamin D regulates inflammatory cytokine production — a lethal hallmark of COVID-19 — and is an important regulator of your immune system. Dysregulation of the immune system is another hallmark of severe COVID-19.
Seheult also reviews studies showing COVID-19 outcomes appear to be linked to UVB exposure. For example, in one such study,11 they found a marked variation in mortality depending on whether the patients lived above or below 35 degrees North latitude. As noted by the authors:12
” … the hypothesis is not that vitamin D would protect against SARS‐CoV‐2 infection but that it could be very important in preventing the cytokine storm and subsequent acute respiratory distress syndrome that is commonly the cause of mortality.”
Now, as noted by Seheult, it’s also possible that COVID-19 itself might be the cause of the lower vitamin D levels seen in these patients. This was reviewed in a letter to the editor, titled, “Vitamin D Deficiency in COVID-19: Mixing Up Cause and Consequence,” published in Metabolism: Clinical and Experimental, November 17, 2020.13 What they found was that as plasma cytokine levels increased in COVID-19 patients, vitamin D levels modestly dropped.
• Vitamin D influences infection risks — Vitamin D has also been linked to a lower risk of testing positive for COVID-19 in the first place.
The largest observational study14 to date, which looked at data for 191,779 American patients, found that of those with a vitamin D level below 20 ng/ml (deficiency), 12.5% tested positive for SARS-CoV-2, compared to 8.1% of those who had a vitamin D level between 30 and 34 ng/ml (adequacy) and 5.9% of those who had an optimal vitamin D level of 55 ng/ml or higher. According to the authors:
“SARS-CoV-2 positivity is strongly and inversely associated with circulating 25(OH)D levels, a relationship that persists across latitudes, races/ethnicities, both sexes, and age ranges.”
How to Improve Your Vitamin D Absorption
The specific dosage required to maintain an optimal vitamin D level can vary widely from person to person depending on a variety of factors, including age and weight. Your gut health can also play an important role in how well you absorb the vitamin D you take, according to recent research.15
When you have a healthy gut, beneficial bacteria produce butyrate by breaking down dietary fiber. Butyrate, in turn, helps increase vitamin D, so the more butyrate you have, the more vitamin D your body can absorb.
Another factor that can influence your vitamin D absorption is your magnesium level.16 Magnesium is required for the conversion of vitamin D into its active form.17,18,19,20 According to a scientific review21,22 published in 2018, as many as 50% of Americans taking vitamin D supplements may not get significant benefit as the vitamin D simply gets stored in its inactive form, and the reason for this is because they have insufficient magnesium levels.
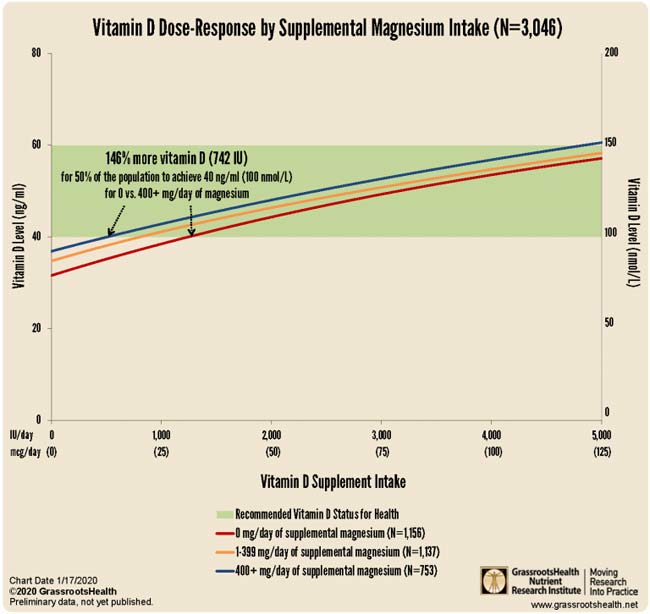
More recent research by GrassrootsHealth23 shows you need 146% more vitamin D to achieve a blood level of 40 ng/ml (100 nmol/L) if you do not take supplemental magnesium, compared to taking your vitamin D with at least 400 mg of magnesium per day.
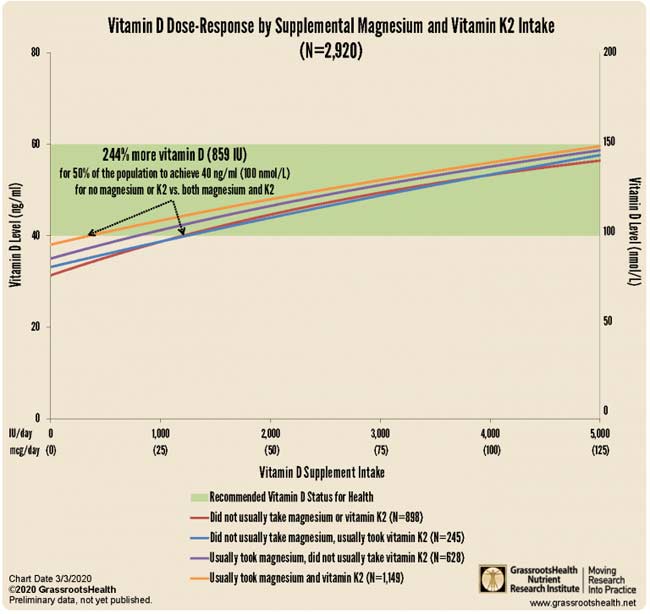
Your vitamin K2 intake can also affect your required vitamin D dosage. According to GrassrootsHealth,24 “combined intake of both supplemental magnesium and vitamin K2 has a greater effect on vitamin D levels than either individually,” and “those taking both supplemental magnesium and vitamin K2 have a higher vitamin D level for any given vitamin D intake amount than those taking either supplemental magnesium or vitamin K2 or neither.”
Data25 from nearly 3,000 individuals revealed 244% more oral vitamin D was required to get 50% of the population to achieve a vitamin D level of 40 ng/ml (100 nmol/L) if they weren’t concurrently also taking magnesium and vitamin K2.
Safeguard Your Immune System With Vitamin D
In summary, if you cannot get sufficient amounts of sun exposure to maintain a vitamin D blood level of 40 ng/mL (100 nmol/L) to 60 ng/mL (150 nmol/L), a vitamin D3 supplement is highly recommended. Just remember that the most important factor here is your blood level, not the dose, so before you start, get tested so you know your baseline.
This will help you determine your ideal dose, as it can vary widely from person to person. Also remember that you can minimize your vitamin D requirement by making sure you’re also getting enough magnesium and vitamin K2. I’m convinced optimizing your vitamin D can go a long way toward minimizing your chances of contracting a respiratory infection, be it the common cold, seasonal influenza or COVID-19.
If you live in the northern hemisphere, now is the time to check your vitamin D level and start taking action to raise it if you’re below 40 ng/mL (100 nmol/L). Experts recommend a vitamin D level between 40 and 60 ng/mL (100 to 150 nmol/L).
An easy and cost-effective way of measuring your vitamin D level is to order GrassrootsHealth’s vitamin D testing kit. Also, if you haven’t already visited www.stopcovidcold.com please do so now so you can take your free COVID risk test and grab a free PDF copy of my vitamin D report.
Once you know your current vitamin D level, use the GrassrootsHealth vitamin D calculator26 to determine how much vitamin D you might need to reach your target level. Retest your vitamin D level in three to four months to make sure you’ve reached your target level. If you have, then you’re taking the correct dosage. If you’re still low (or have reached a level above 80 ng/mL), you’ll need to adjust your dosage accordingly and retest again in another three to four months.
[ad_2]
Source link