[ad_1]
AsianScientist (Apr. 2, 2021) – On the second to the last day of an extremely challenging 2020, Singapore opened a bright new chapter in its fight against the pandemic. That day, senior staff nurse Sarah Lim became the first person in Singapore to receive a COVID-19 vaccine, ahead of 39 other colleagues at the National Centre for Infectious Diseases, a frontline healthcare institution caring for COVID-19 patients.
The fact that vaccines were being administered less than a year after the disease first landed on Singapore’s shores is an amazing achievement and a testament to human ingenuity. Yet what is a scientific marvel for some has proven to be a source of suspicion for others, who question if the speed at which the vaccines were approved has somehow short-circuited the typically rigorous approval process.
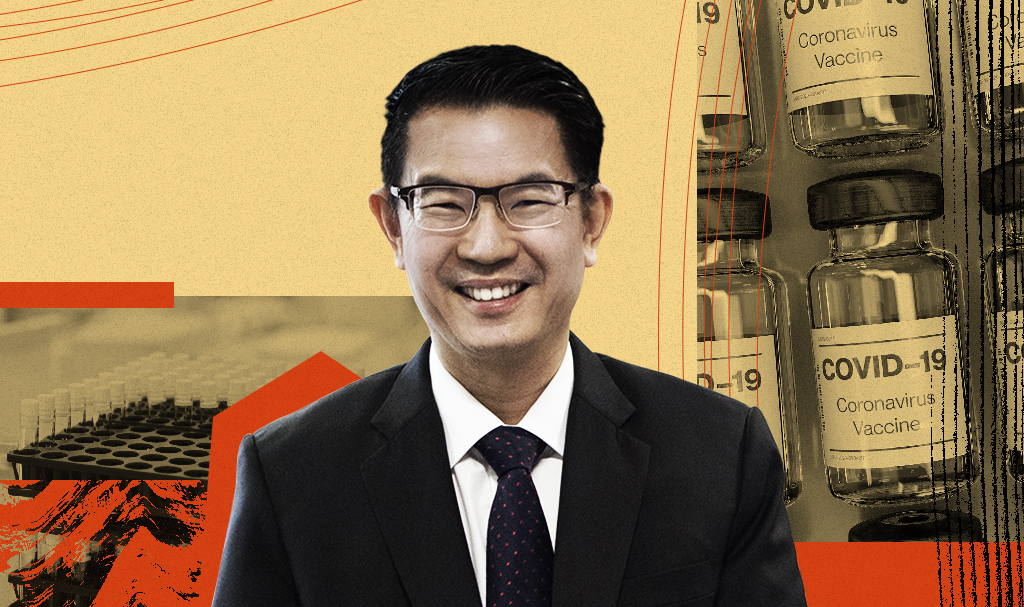
The answer is a categorical no, says Professor John Lim, founding executive director of the Centre of Regulatory Excellence (CoRE) at Duke-NUS Medical School. According to Lim, both the Pfizer-BioNTech and Moderna vaccines—which were granted interim approval on Dec 15, 2020 and Feb 2, 2021, respectively—have met all requirements for safety, efficacy and quality as demanded by the Health Sciences Authority of Singapore (HSA) under its Pandemic Special Access Route.
“Simply because HSA calls it an interim authorization doesn’t mean that they think it is less safe,” said Lim, who was CEO of HSA for eight years from 2006 to 2014. In fact, with over a million doses administered in Singapore adding to the 565 million doses administered worldwide, it is safe to say that any significant adverse effects for these vaccines would have been picked up by now, he added. “The safety profile based on the many people vaccinated to date is very reassuring.”
In this interview with Asian Scientist Magazine, Lim explains how the approval of the COVID-19 vaccines was expedited and how decades of work behind the scenes have positioned regulators to respond both rapidly and rigorously to outbreaks.
Q: What do regulators look for when deciding whether or not to approve a new vaccine?
The three basic tenets of any regulatory approval are safety, efficacy and quality. For any product, these three things must always be assured by any national regulatory authority; and it certainly continues to apply in the case of vaccines.
During the different phases of clinical trials—whether phase 1, 2 or 3—the key thing that they will be looking for in terms of safety is common adverse events. Normally, even in a phase 3 trial, you would be looking at between 3,000 to 5,000 subjects. The Pfizer-BioNTech vaccine, for example, was trialed on over 43,000 people, so one is much more assured that any significant adverse events would have been picked up.
This is why the Singapore government and others are confident in saying that the safety profile of the vaccine is very good. Even so, we will continue to track it because what has been given to the Pfizer-BioNTech and Moderna vaccines are interim authorizations, or what is called emergency use authorization in other jurisdictions.
However, it is important to note that that an interim authorization doesn’t mean it is less safe. To complete the process, the regulators are asking the vaccine manufacturers to continue giving further information for one or two years before converting the approval to full authorization. And that is good because it commits companies to post-approval monitoring, which would normally be called post-marketing approval or phase 4 trials, although the terminology doesn’t quite apply in this case.
The second tenet is efficacy, or the extent to which a vaccine provides a beneficial result under ideal conditions and is usually measured in phase 3 trials. But then there is the other aspect of effectiveness, which is the extent to which a vaccine provides a beneficial result under real life conditions. This is usually tracked as the programs are being rolled out.
Last but not least, quality is essential because you want to guarantee a high degree of consistency in terms of the product. Controlling the manufacturing site and process ensures the quality and purity of the starting materials. What’s also important is that there are controls in the manufacturing process to confirm the quality of the process, which is an essential point of a good manufacturing practice.
The other thing is if there are validated process procedures, they must be adhered to so that the processes are not just on paper, but actually happening in practice. Inspectors will check on the more established pharmaceutical companies routinely, so there is a greater assurance that these processes are in place. Smaller biotech companies typically link up with a larger pharmaceutical company to ensure that this manufacturing quality process is followed.
Q: Why were the regulators able to approve the COVID-19 vaccines so quickly?
If you look at the global situation and what other regulatory agencies have done, it is quite extraordinary how fast the process has been. Nonetheless, there has been no reduction in the quality and robustness of the assessment. This is because regulators around the world have been in constant communication with each other throughout the pandemic, building on efforts that began 10 to 15 years ago.
For example, the International Coalition of Medicines Regulatory Authorities (ICMRA) went into a very intensive series of nearly fortnightly discussions in response to COVID-19, where they were convening virtual meetings and getting the latest updates on the various technical scientific issues that feed into regulation. That sharing of information has been very critical in expediting the approvals.
The key thing here is that each regulator must take into account the dossier that is submitted to them, in this case, on a rolling submissions basis because of the speed at which information was coming through. But because regulators were able to cross reference with each other, we can be assured that there’s a great deal of robustness in the process; it’s not just every regulator making its own decisions in isolation.
Q: Apart from the urgent re-prioritization, what other factors helped expedite vaccine approvals?
One thing that helped was the fact that rolling submissions are not new and have been talked about for the past ten years. HSA was actually one of the earlier organizations looking into such a process, where you do not necessarily wait for the sequential phases of data but overlap the phases so that you can collect the data faster. At the time, there was more conservatism about actually applying it, mainly because it was not the way things were done in the past. But because people have previously thought through what a rolling submission is and what it means, it was not such a big leap to actually do it when the situation called for it.
The vaccines themselves are also based on a known technology. Although they are described as new in the sense of being used as a vaccine, people have actually been looking at mRNA technology for more than ten years in the oncology space. If it were really completely new and we knew nothing about the underlying technology, I think you would not have seen the speed we witnessed, especially for the Pfizer-BioNTech and Moderna products that were given emergency authorization.
Q: Now that we know that it is possible to get a vaccine approved in under a year, how does this change the regulatory landscape in Singapore?
The speed at which we were able to approve the COVID-19 vaccines leads to your next question: What is the potential longer-term impact on regulations in general? I think it will be a positive one. We are advocating that all these good practices that have resulted from COVID-19 should form a ‘new normal’ for regulations going forward. Not just because there may be yet another public health emergency down the road, but the same could also apply for access to new therapies.
Like moving from working in the office to working from home, most organizations think it is a good idea to implement measures like rolling submissions. The pandemic has shown regulators that it can work, although it does require some rejigging of priorities and the way in which staff are organized. With the processes now in place, they can definitely be re-used.
Having said that, we don’t want to throw the baby out with the bathwater and swing to the other extreme. There should be some prioritization of which products you would apply this to because it requires refocusing resources, and every agency will have a limitation on its number of people. Even for rolling submissions, you would not necessarily want to do that in every situation. Everything has to be balanced because you’re looking at public health and safety, and you want to be sure that the decisions taken are very sound and evidence-based.
———
Copyright: Asian Scientist Magazine; Photo: Duke-NUS Medical School.
Disclaimer: This article does not necessarily reflect the views of AsianScientist or its staff.
[ad_2]
Source link